Serotonin Hypothesis
For the last half-century, the dominant explanation for depression has centered on [...]
Sylvia Plath
Born on October 27, 1932, in Boston, Massachusetts, Sylvia Plath [...]
GLP-1 Antagonist Drugs for Anxiety & Depression
In the "South Park" special titled "The End of Obesity," [...]
Understanding The Human Brain
Thoughts, memories, sensations — why are we still in the [...]
Amazing Listeners
Like bees to bright, we are naturally drawn to amazing [...]
TF-CBT
Child trauma is a serious societal problem. At least one [...]
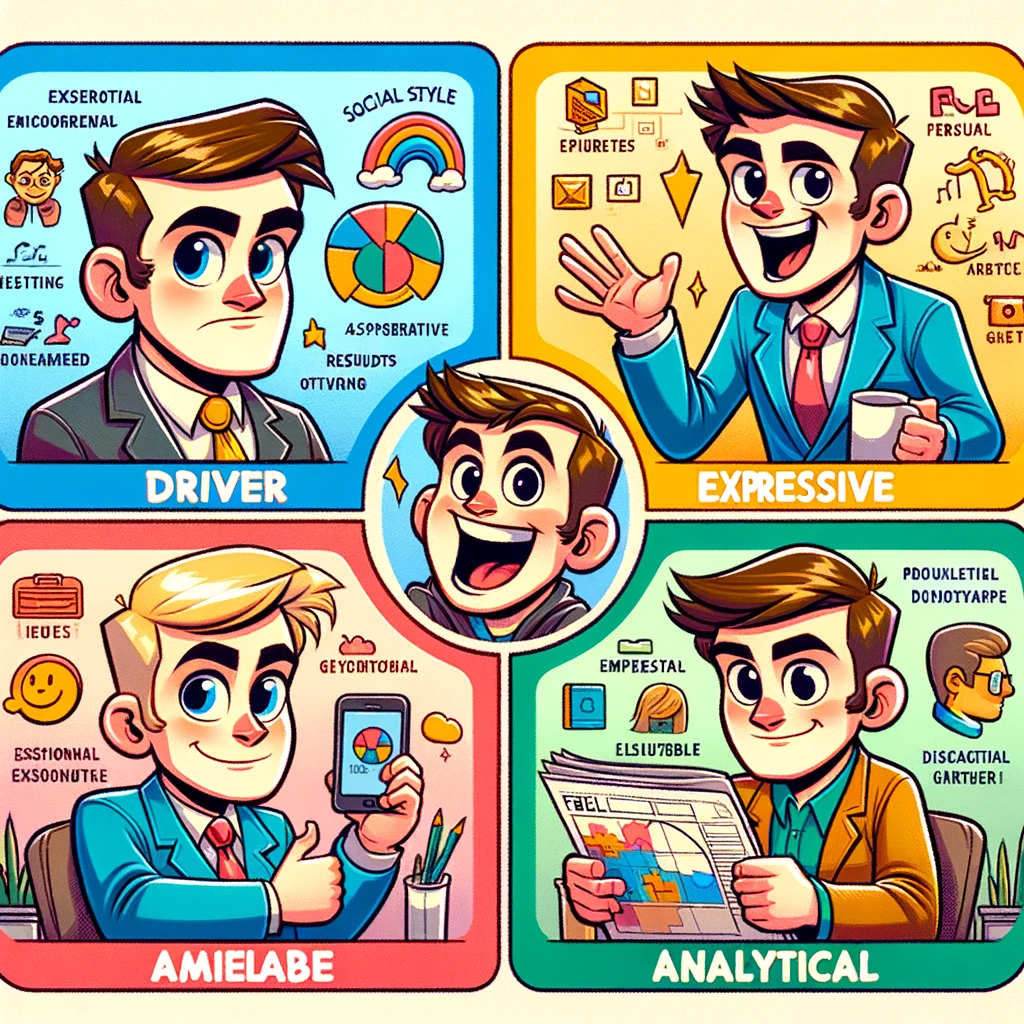
Social Styles Model
Do you pay attention to what is happening when other [...]
Clinical Hypnosis
With decades of data and new research supporting its effectiveness, [...]
Mentally Healthy
Some of us have grown up in families where negativity, [...]
Journaling For Self-Care
If you are the caregiver in a relationship, it can [...]